What is Mohs surgery?
FAQs
-
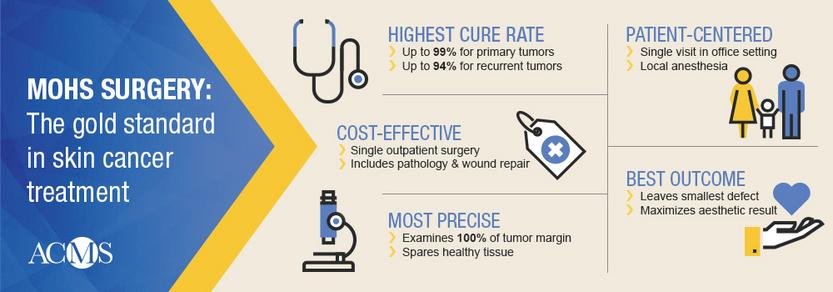
Mohs surgery, also known as Mohs micrographic surgery, is a specialized surgical procedure used to treat certain types of skin cancer, particularly basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). It is named after the surgeon who developed the technique, Dr. Frederic Mohs.
How Mohs Works:
Removal: The Mohs surgeon removes the visible tumor (indicated by the biopsy report) along with a thin 1 - 2 mm margin layer of surrounding tissue.
Microscopic Examination: The removed tissue is carefully mapped, and the Mohs surgeon examines the edges of the tumor under the microscopic in the in-house laboratory. This process takes anywhere between 1 — 2 hours and allows the surgeon to check if any cancer cells remain in the margins of the excised tissue.
Final Results: The removal and examination process is repeated layer by layer until no cancerous cells are detected at the margins. The wound is then repaired, or in certain scenarios, left to heal on its own.
One of the benefits of Mohs surgery is that the procedure preserves as much healthy tissue as possible, thereby minimizing scarring and reducing the risk of recurrence. Overall, it is a highly effective option for treating skin cancers; it is the current gold standard of care.
-
Some of the indications for Mohs surgery include the following:
High-Risk Cancers: Skin cancers located in areas where cosmetic appearance is important, such as the face, ears, nose, or around the eyes.
Large, Aggressive, or Recurrent Tumors: The procedure is particularly effective for skin cancers that have been previously treated in a variety of ways and come back.
Rare tumors: In additional the three common tumors for which Mohs surgery is used, such as squamous cell carcinoma, basal cell carcinoma, and melanoma, Mohs surgery can be used to treat rare tumors such as dermatofibrosarcoma protuberans and microcystic adnexal carcinoma.
Tumors in patients with a weakened immune system: Patients who are immunocompromised such as those taking immunosuppressive medications for an organ transplant are at a higher risk of skin cancer and these cancers tend to be more aggressive and harder to treat.
-
Mohs surgery has a high success rate because it checks for remaining cancerous cells immediately. The procedure is done in quick sessions, meaning patients undergo skin cancer removal and reconstruction on the same day.
Because minimized areas are removed in each stage, healthy tissue is preserved at a higher rate, resulting in less scarring compared to other forms of treatment.
-
In certain situations, Mohs surgery can be used to treat early stage melanoma that is confined to the skin’s outer layers, especially if the melanoma is located in a cosmetically sensitive area. Melanoma treated with Mohs surgery and the MART-1 immunostain, a special dye used to evaluate tissue margins, has a cure rate of up to 99%.
Dr. Terushkin’s repertoire includes surgical and pathological training for the treatment of melanoma using Mohs. He is the first Mohs surgeon in New York City to have treated melanoma with Mohs surgery and the MART-1 immunostain.
-
Although it is generally considered safe and effective, Mohs surgery carries some risk (as does any surgical procedure). The risks are relatively low:
Infection: Because the skin is an external surface exposed to bacteria, there is a small risk of infection. Mohs surgeons use sterile techniques and give specific wound care instructions to reduce the risk of infection.
Bleeding: The removal of tissue can lead to bleeding. Patients who take blood thinners may be more prone to bleeding. Please note that blood thinners are not stopped during the procedure.
Scarring: Although Mohs is known to minimize scarring, any surgical procedure leaves a scar. See the next tab for more information about scarring.
Pain or Discomfort: Though Mohs is generally well-tolerated, some pain or discomfort may occur. Local anesthesia is used during the procedure to numb the area, and post-procedure discomfort can be managed with Tylenol and/or Advil.
Nerve Damage (Rare): If a skin cancer is located near a nerve, there is a small risk of nerve damage that could result in numbness, tingling, or muscle weakness. Mohs surgeons take care to avoid damaging nerves; most damage is temporary.
Overall, Mohs is a highly effective, safe, and minimally invasive procedure. The cure rate is 97 — 99%. The risks associated with Mohs are relatively low, but are still important to consider. Proper wound care can help minimize the risks and ensure the best possible outcome. If you have more concerns, please discuss with them with our team at the time of your appointment.
-
The approach to taking care of the wound depends on a number of factors, including the size of the wound, depth of the wound, location of the wound, and other patient characteristics. Some wounds are left to heal on their own while others can be closed in a line. Other times, we may need to borrow skin from another location to patch up the wound. That is called a skin graft. We are also trained to perform skin flaps, which means moving skin adjacent to the wound to cover up the wound. Finally, we sometimes work with other specialists to help close the wound.
As with any surgical procedure, Mohs surgery reconstruction will leave a scar. The extent of scarring depends on numbers factors. In some situations, the wound may take longer to heal than expected, especially if the skin cancer was large or located on the lower extremity.
-
Mohs surgery is the standard of treatment for the removal of skin cancers. The procedure has the highest cure rates, particularly with cancers with a high risk of recurrence or in difficult-to-treat or sensitive areas like the face.
The cure rate for Mohs is > 99% for new skin cancers and around 95% for recurrent cases.
What will the day of my appointment look like?
-
Here’s a guide to help you get ready for your Mohs surgery:
Confirm Details: Make sure you have an understanding about the type of skin cancer you have. You must be able to identify the exact site that needs to be treated, so if you are unsure, confirm with your dermatologist in advance. Be sure to ask any questions you have.
Dress Comfortably: Wear loose, comfortable clothing. Avoid wearing white clothing and makeup. We will have you change into a surgical gown if we need access to a site on the body.
Bring Something to Do: Mohs surgery can take anywhere from 2 hours to a full day. After each layer of tissue is removed, you will sit in the waiting room while the results are examined. Bring a book, tablet, or smartphone to keep yourself occupied. We have free Wifi and charging access.
-
For non-melanoma skin cancers being treated with Mohs, please expect to be at the office for half a day.
For melanoma skin cancers, please set aside a full day for the procedure.
-
Unless otherwise advised, you can eat before Mohs surgery.
-
Unless specifically instructed, we do not routinely request that you stop any medications, including blood thinners, prior to your procedure.
-
Unless otherwise advised, you do not need a chaperone for this appointment. Many patients transport themselves to and from our office without aid; however, if you would like company, you may bring one person with you. Due to limited space in the office, we ask that you adhere to this guideline.
-
In most cases, you can drive after having Mohs. We use local anesthesia to temporarily numb the area, meaning that you will be awake during the procedure. Since local anesthesia doesn’t affect your ability to think clearly or cause drowsiness, it’s generally safe to drive once the procedure is over if you feel comfortable.
If you are feeling uncertain, tired, or experience any discomfort, it’s best to have a chaperone assist you.
Other Common FAQs:
-
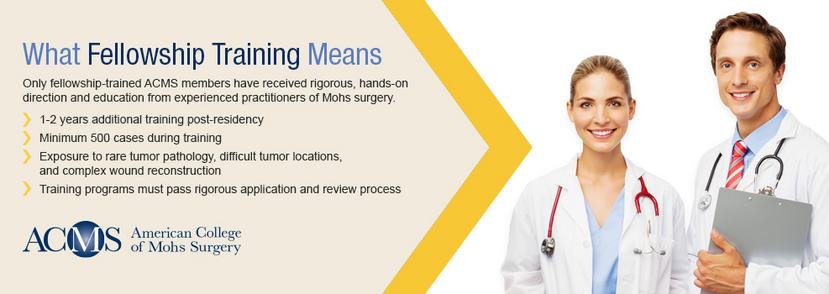
A fellowship trained Mohs surgeon has undergone additional, specialized training beyond their general dermatology residency. The Mohs surgery fellowship is a post-residency, advanced training program that provides specific education focusing on Mohs micrographic surgery and cutaneous oncology.
In their fellowship year, Mohs surgeons learn how to do the Mohs micrographic surgery, microscopic evaluation, and reconstructive surgery. During training, Mohs surgeons perform numerous Mohs procedures under the supervision of an experienced Mohs surgeon and pathologist to develop a high level of proficiency and an understanding of the nuances of skin cancer behavior. Training also equips surgeons with advanced techniques for reconstructive procedures.
Fellowship training is conducted through accredited programs that are recognized by the American College of Mohs Surgery. Dr. Terushkin completed his fellowship under the supervision of Dr. Zitelli and Dr. Brodland in Pittsburg, and Dr. Becker completed his at Mass General Hospital.
Why fellowship training matters:
Expertise: Fellowship trained Mohs surgeons are among the most highly skilled in the field of skin cancer surgery.
Higher success rate: Fellowship trained surgeons are generally more adept at achieving clear surgical margins, minimizing the risk of recurrence, and performing cosmetically favorable reconstructions.
-
A board-certified Mohs surgeon has met the rigorous standards set by a recognized medical board to specialize in Mohs micrographic surgery.
A Mohs surgeon has:
Specialized Training: The Mohs surgeon has completed a 1 - 2 year fellowship in Mohs surgery, learning the precise removal of skin cancers and microscopic examination of tissue.
Certification: After fellowship, the Mohs surgeon can pursue additional certification from the American College of Mohs Surgery and the American Board of Dermatology. This process involves completing additional training, demonstrating competency in the field, and passing board exams.
-
The difference between Mohs surgery and a surgical excision lies in the technique used to remove the skin cancer and the overall precision of the procedures.
Mohs is a layer-by-layer technique that preserves tissue on delicate areas of the body. Mohs surgery allows for 100% margin control, meaning that the surgeon can ensure that all cancer is removed before the wound is closed, surgically or naturally. This is important for skin cancers in areas with complex anatomy or a high risk of recurrence. The cure rates from Mohs are over 95 - 99%.
A surgical excision is a more traditional method for removing skin cancers and can used for a wider variety of tumors. The surgeon removes the tumor with a single excision that includes the cancerous tissue and a larger surrounding margin and sutures the wound immediately. The tissue is then sent to a laboratory for pathological examination, which can take up to a week. A surgical excision is typically quicker than Mohs because it does not involve real-time microscopic analysis. While it is highly effective, the cure rate is generally lower than Mohs. In addition, the scar may be larger than with Mohs surgery, especially because the margin of healthy tissue removed is significantly larger than in Mohs.
-
-
There are several other treatments for skin cancer, typically reserved for patients who are not good candidates for Mohs surgery:
Cryotherapy: This technique, freezing the skin cancer with liquid nitrogen, is best for superficial pre-cancers. It is minimally invasive and quick, but is not effective for larger or deeper skin cancers.
Topical Treatments: Topical chemotherapy creams are good for treating pre-cancers. However, they can cause redness, irritation, or ulceration at the treatment site.
Photodynamic Therapy (PDT): This technique involves using a photosensitizing drug and a light source that activates the drug to destroy cancer cells. While less invasive than Mohs surgery, it is less effective and may cause redness and photosensitivity.
Electrodesiccation and Curettage (ED&C): The tumor is scraped off using a curette, which is simple, quick, and effective for small, superficial BCCs and SCCs. It is not ideal for deeper or larger cancers.
Systemic Treatments (Chemotherapy/Immunotherapy): Chemotherapy can be used for advanced/metastatic SCCs or metastatic melanomas. Immunotherapy is a newer treatment approach used primarily for melanoma. Both treatments can result in larger, systemic symptoms such as immune weakness, inflammation, nausea, fatigue, and hair loss.
Choosing the best treatment type depends on the type of skin cancer, size and location, the health of the patient, and cosmetic considerations. Mohs surgery is the standard of care for removing BCCs, SCCs, and early stage melanomas.
-
For questions regarding insurance, please contact our office at (212) 772-3600.